WHY DO YOU WANT TO TEST MY PETS BLOOD?
Like us, our pets can suffer from metabolic anomalies too! Their organs can fail, and they can run out of natural ability to clot the same way we can. Routine blood screening can assist us with defining issues before they become major emergencies. Especially prior to surgery!
COMPLETE BLOOD COUNT (CBC)
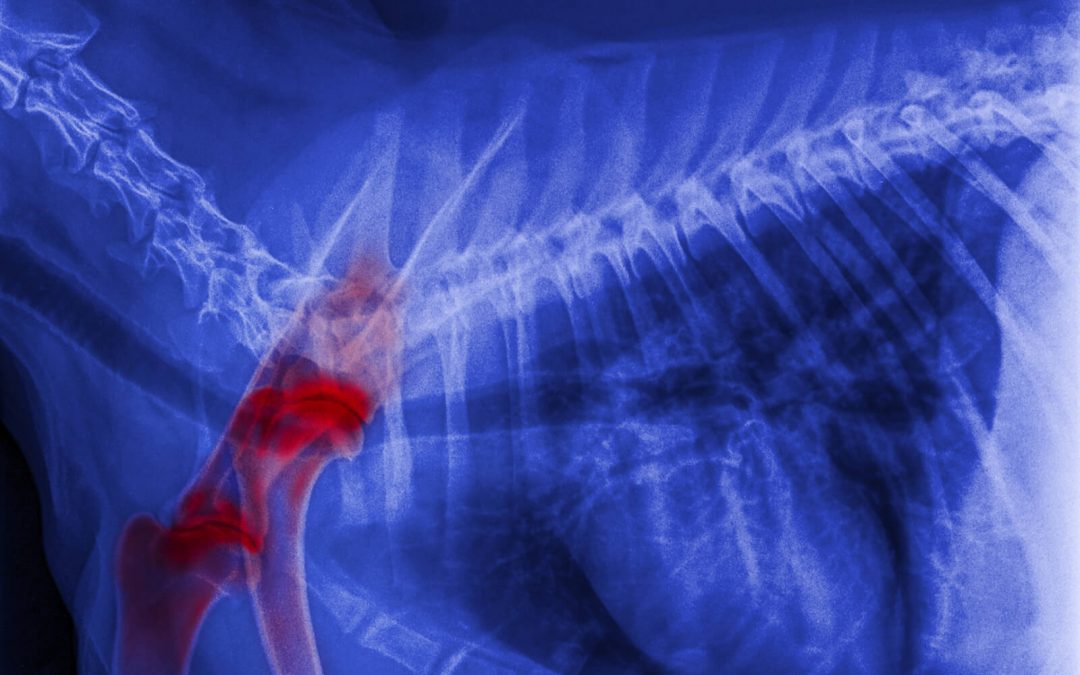
This is the most common blood test performed on pets and people. A CBC gives information on hydration status, anaemia, infection, the blood’s clotting ability, and the ability of the immune system to respond. This test is essential for pets with fevers, vomiting, diarrhoea, weakness, pale gums, or loss of appetite. If your pet needs surgery, a CBC can detect some bleeding disorders or other unseen abnormalities.
Red Cell Count measures the total number of red blood cells per volume of blood. It is used in detecting anaemia and other disorders of red blood cells. MCV (Mean Cell Volume) measures the volume of the individual red blood cell.
- Haemoglobin is the oxygen-carrying pigment of red blood
cells. MCHC and MCH (mean corpuscular haemoglobin concentration and mean corpuscular haemoglobin) are all measures of haemoglobin and used in differentiating some anaemias.
- PCV (packed Cell Volume or haematocrit) measures the percentage of red blood cells to detect anaemia and dehydration.
White Cell Count (white blood cell count) measures the body’s immune cells. Increases or decreases may indicate certain diseases, infections or inflammation.
- Neutrophils, lymphocytes and monocytes are specific types of white blood cells. Disturbances of these may indicate infection, stress, cancer, hormonal imbalances and other conditions.
- Eosinophils are a specific type of white blood cell that may indicate allergic or parasitic conditions.
Platelet count measures cells that help to form blood clots.
Reticulocytes are immature red blood cells. High levels indicate rebuilding of red blood cell numbers.
BLOOD CHEMISTRIES
These common blood serum tests evaluate organ function, electrolyte status, hormone levels and more. They are important in evaluating older pets, pets with vomiting, diarrhoea or toxin exposure, pets receiving long-term medications and health before anaesthesia.
- Na (sodium) is an electrolyte lost with vomiting, diarrhoea, kidney disease and Addison’s disease. This test helps indicate hydration
- K (potassium) is an electrolyte lost with vomiting, diarrhoea or excessive urination. Increased levels may indicate kidney failure, Addison’s disease, dehydration or urethral obstruction. High levels can lead to a heart
- Cl (chloride) is an electrolyte often lost with vomiting and Addison’s disease. Elevations often indicate
- Bicarb is an indication of acid / base balance and can be changed with vomiting and other conditions.
- BUN (blood urea nitrogen) indicates kidney function. An increased level in the blood is called azotaemia and can be caused by kidney, liver, heart disease, urethral obstruction, shock and
- CREA (creatinine) reveals kidney function. This test helps distinguish between kidney and non-kidney causes of elevated BUN
- Ca (calcium) deviations can indicate a variety of diseases. Tumours, hyperparathyroidism, kidney disease and low albumin are just a few of the conditions that alter serum
- PHOS (phosphorus) elevations are often associated with kidney disease, hyperthyroidism and bleeding
- AMYL (amylase) elevation may indicate pancreatitis or kidney
- LIP (lipase) is an enzyme that may indicate
- TP (total protein) indicates hydration status and provides additional information about the liver, kidneys and infectious
- ALB (albumin) is a serum protein that helps evaluate hydration, haemorrhage, intestinal, liver, and kidney
- GLOB (globulin) is a blood protein that often increases with chronic inflammation and certain disease states, including some
- TBIL (total bilirubin) elevations may indicate liver or haemolytic This test helps identify bile duct problems and certain types of anaemia.
- ALKP (alkaline phosphatase) elevations may indicate liver damage, Cushing’s disease or active bone growth in young This test is especially significant in cats.
- ALT (alanine aminotransferase) is a sensitive indicator of active liver damage but doesn’t indicate the
- GGT (gamma glutamyl transferase) is an enzyme that indicates liver disease or corticosteroid excess.
- AST (asparate aminotransferase) increase may indicate liver, heart or skeletal muscle damage.
- CK (Creatine Kinase) is an enzyme that indicates muscle
- LDH (Lactic Rehydrogenase) is an enzyme that can be elevated in muscle, heart and liver
- CHOL (cholesterol) is used to aid in the diagnosis of hypothyroidism, liver disease, Cushing’s disease and diabetes
- GLU (glucose) is a blood sugar. Elevated levels may indicate diabetes Low levels can cause collapse, seizures or coma.
- Cortisol is a hormone that is measured in tests for Cushing’s disease (the low- dose dexamethasone suppression test) and Addison’s disease (ACTH stimulation test)
- T4 (thyroxine) is a thyroid hormone. Decreased levels often signal hypothyroidism in dogs, while high levels may indicate hyperthyroidism in